
Our Project ECHO® work is an important part of our Center’s portfolio. The Project ECHO Model® was developed by the ECHO Institute at the University of New Mexico. ECHO participants engage in a virtual community of practice with their peers where they share support, guidance and feedback in an all teach, all learn framework. The Model allows for the dissemination and implementation of best practices across diverse disciplines and professions to continuously improve care for patients, especially those residing in rural or underserved communities. During an ECHO session, in addition to didactic education, participants present anonymized real cases to the specialists—and each other—for discussion and recommendations. The extended and continuous loop of learning, mentoring, peer support, and multidisciplinary and interprofessional expert and participant teams’ holistic approach is what makes ECHO both robust and unique and provides a long-lasting impact.
To date, we have sponsored ECHO programs on the topic of Huntington’s Disease, Short Bowel Syndrome, Autism, Fetal Alcohol Spectrum Disorders (FASD), Addiction Medicine, and Migraine QI. The multi-state, multi-year HRSA funded ECHO on Fetal Alcohol Spectrum Disorders under the direction of Daniel Alford, MD has run three cohorts, and each cohort includes two series, one for maternal child health clinicians (family medicine and OB/GYN) and one for pediatric care clinicians. Initial outcomes were presented at the 2022 Annual Meeting of AMERSA, as well as at Together for Hope Boston Addiction Conference (2024) and the annual meeting of the Canada FASD Research Network (2024). A five-year grant proposal for a national expansion of this program was approved by HRSA in 2024.
We are also working with Dr. Alford on an ECHO series created to teach faculty how to design, implement, and evaluate an addiction medicine curriculum in their institutions. This five-year, NIDA-funded program ran its first cohort June 2023 through February 2024. Initial outcomes were presented at the Together for Hope Boston Addiction Conference and at the 2024 Boston University Chobanian & Avedisian School of Medicine’s John McCahan Day in 2024. The second cohort began in June 2024.
The CCE team, in partnership with Clinical Care Options, launched a 12-month Migraine ECHOQI program which started in September of 2023 with 13 neurology practices from the East Coast, South and Midwest. The ECHO addressed migraine prevention and focused on training community neurology practices in quality improvement methods through conducting individual QI projects with the goal of reducing migraine days. Aims for the projects included increasing patient counseling on at least one modifiable lifestyle or chronification factor during the measurement period or increasing the number of eligible patients appropriately prescribed a preventive migraine therapy. The ECHO sessions addressed QI methods, the participants’ experience conducting their QI projects and clinical care to prevent migraine.
The participating sites implemented interventions related to patient education, optimizing prior authorization processes, lifestyle referrals, appointment and intake scripting, updating data collection, and implementing telemedicine follow-ups to improve access. Preliminary results indicate that six out of ten sites which completed the ECHO reported a reduction in headache burden following their involvement in the ECHO program. While final results are pending, the program shows early signs of success in enhancing clinical outcomes and fostering QI skills in community settings. Final data will be available by the end of 2024. The initiative also includes an on-demand internet activity addressing the experience and results that will launch at the end of 2024.
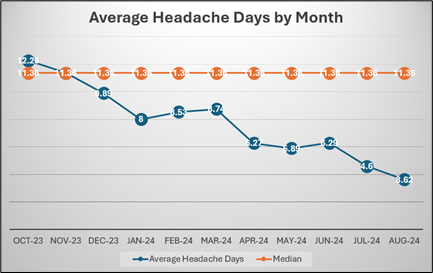
Figure 1: Participating Site 1 run chart showing a shift in the outcome measure indicating statistically significant improvement in average headache days
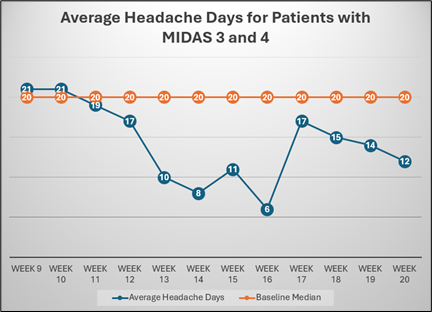
Figure 2: Participating site 2 run chart showing a shift in the outcome measure indicating statistically significant improvement in average headache days for those patients who were most severe (MIDAS 3 and 4 upon start of the initiative).

 Facebook
Facebook X
X LinkedIn
LinkedIn Forward
Forward